Scientific Publication
Proven by science, published worldwide
20 years of clinical validation
Extensive research confirms what surgery has already proven: the aortic ring works, and even better.
Since the first implantation in Paris in 2003, over 80 surgeons in Europe and North America have successfully used the ring in more than 3,500 cases.
These operations have led to numerous scientific publications in international journals confirming the safety, efficacy, and
superiority of this approach compared to valve replacements.
Below you will find the key publications, each accompanied by a simplified summary and a link to the original article.
Validated Excellence
Many international journals have published studies validating the clinical results of the ring.
International Adoption of the Technique
Over 80 surgeons have used the ring, proving its reproducibility and reliability in real-world settings.
Proven Efficacy
Data shows superior life expectancy, fewer complications, and a better quality of life compared to mechanical valves.
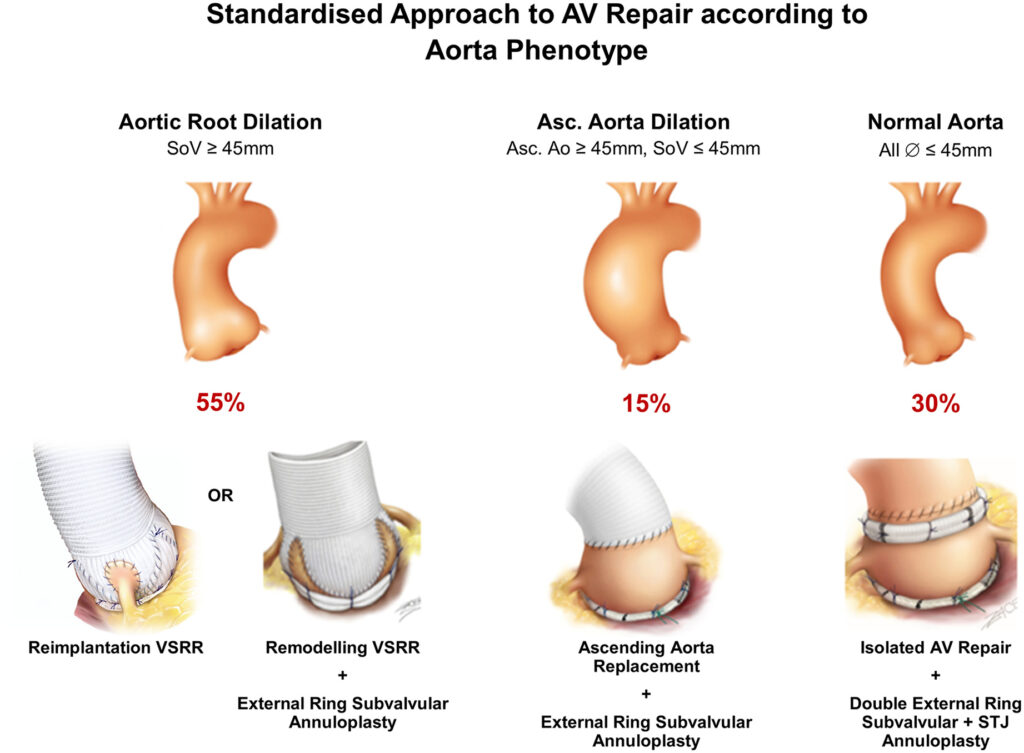
Standardized Aortic Valve Repair
Aortic valve repair has now demonstrated, through long-term data, that it reduces valve-related mortality while restoring a quality of life and life expectancy similar to that of the general population. However, the repair rate remains low worldwide (approximately 15–20%), whereas 80% of regurgitant valves can be repaired. The most common cause of aortic insufficiency (AI) in the West is dystrophic AI, with thin and pliable tricuspid, bicuspid, unicuspid, or quadricuspid valves. Three aortic phenotypes can be distinguished: aortic root dilation; ascending aorta dilation; and isolated AI. Characteristic lesions leading to dystrophic AI include: a dilated annulus > 25 mm, sinotubular junction (STJ) dilation, and cusp prolapse. Sub- and supravalvular aortic annuloplasty (annular reduction), restoration of the annulus-STJ relationship, and resuspension of the effective cusp height are all essential elements of aortic valve repair and valve-sparing aortic root surgery. These procedures increase the cusp coaptation surface and protect the repair for long-term durability.
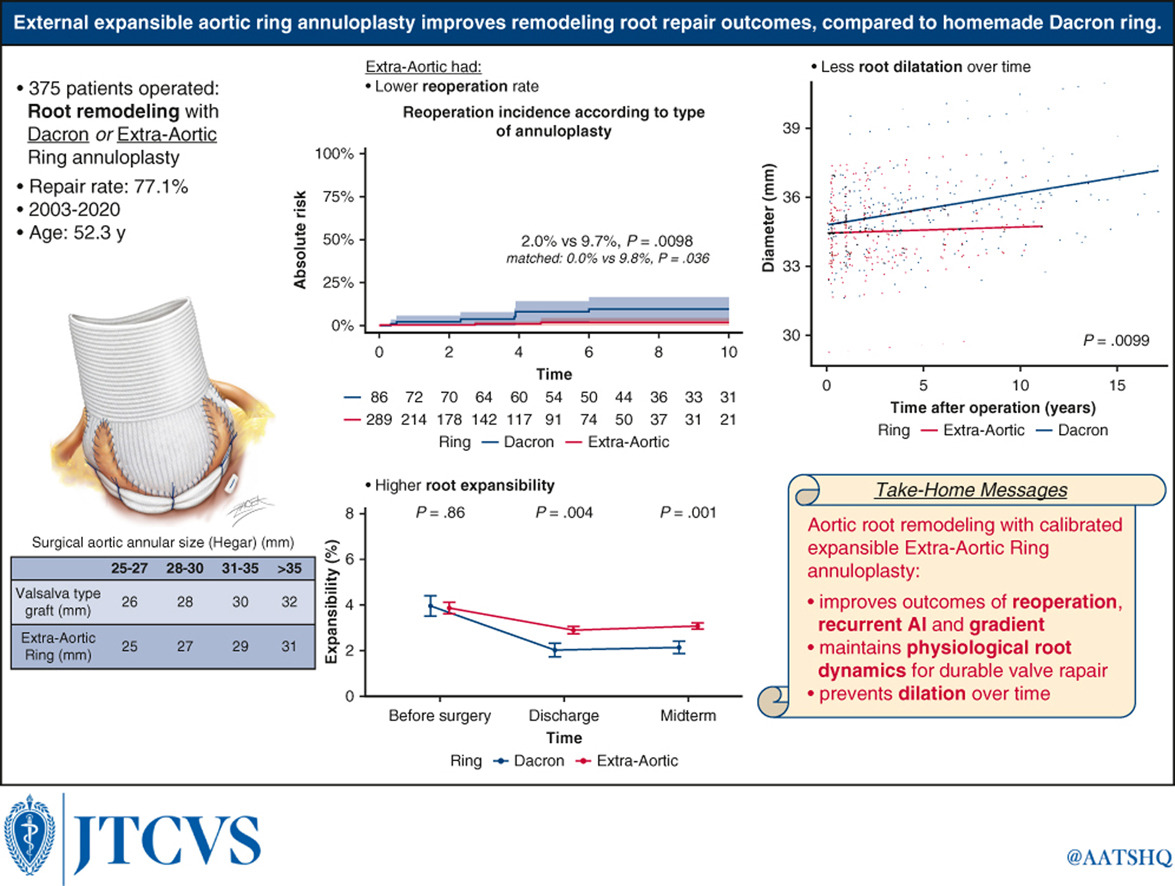
External Aortic Annuloplasty with a Dedicated Expandable Ring Improves Outcomes of Remodeling Root Repair Compared to Hand-Sewn Dacron Ring
Objectives
In valve remodeling with external annuloplasty, we compare the long-term outcomes of a calibrated expandable extra-aortic ring with those of a hand-sewn Dacron ring.
Methods
All patients (2003-2020) who underwent surgery for root aneurysm with or without aortic insufficiency (AI) were included.
The standardized CAVIAAR (Conservation Aortique Valvulaire dans les Insuffisances Aortiques et Anévrysmes de la Racine) technique consisted of root remodeling and external annuloplasty using an extra-aortic ring or a hand-sewn Dacron ring.
Results
Among 486 patients (mean age 52.3 ± 14.0 years) who underwent surgery for root aneurysm, 375 (repair rate: 77.1%) underwent root remodeling with annuloplasty (extra-aortic ring, n = 289, vs. Dacron ring, n = 86).
At 10 years (median follow-up: 4.08 years; interquartile range: 1.95-7.61), unmatched and matched analyses showed that patients with an extra-aortic ring had higher survival, comparable to that of the general population (93.3% vs 79.9%, P = 0.097), a lower incidence of reoperation (2.0% vs 9.7%, P = 0.0098) and a lower recurrence of grade AI >2 (1.9% vs 11.2%, P = 0.0042), compared to patients with a Dacron ring.
The mixed-effects model showed that with extra-aortic ring annuloplasty, annular dilation over time (P = 0.0033) was prevented and, compared to the hand-sewn Dacron ring, root expansibility was better preserved (3.22% vs 2.12%, P = 0.002) and the mean transvalvular gradient was lower (6.58 mmHg vs 7.94 mmHg, P = 0.001).
Tricuspid and bicuspid valves with an extra-aortic ring showed similar reoperation rates (4.3% vs 0.85%, P = 0.65) and AI incidence >2 (2.7% vs 1.2%, P = 0.61), as well as comparable expansibility (P = 0.29) and diameter (P = 0.47), while the mean transvalvular gradient was lower for tricuspid valves (5.58 mmHg vs 7.60 mmHg, P = 0.004).
Conclusions
Valve remodeling with calibrated expandable extra-aortic ring annuloplasty improves outcomes in terms of reoperation and AI recurrence compared to a hand-sewn Dacron ring. It prevents dilation and maintains the physiological dynamics of the root for durable valve repair.
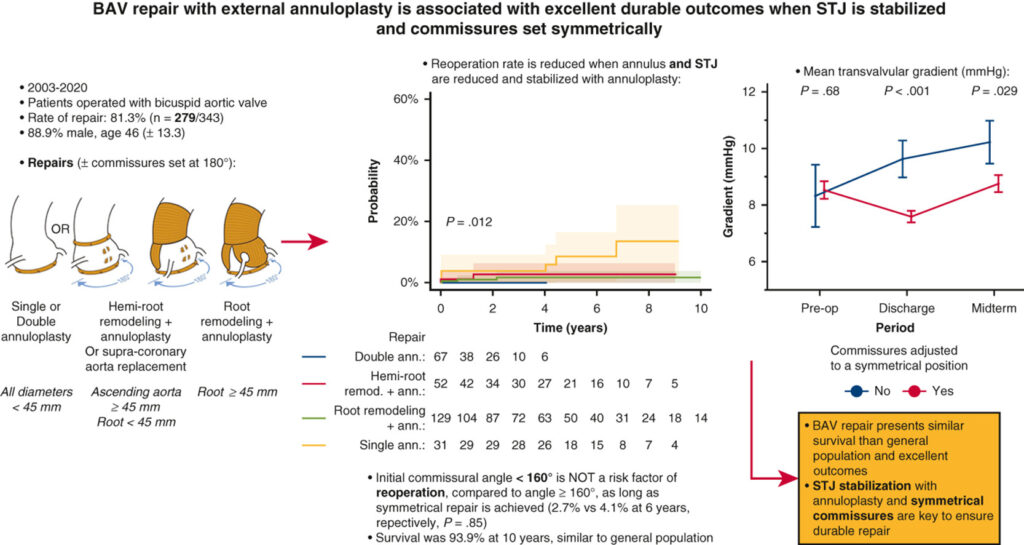
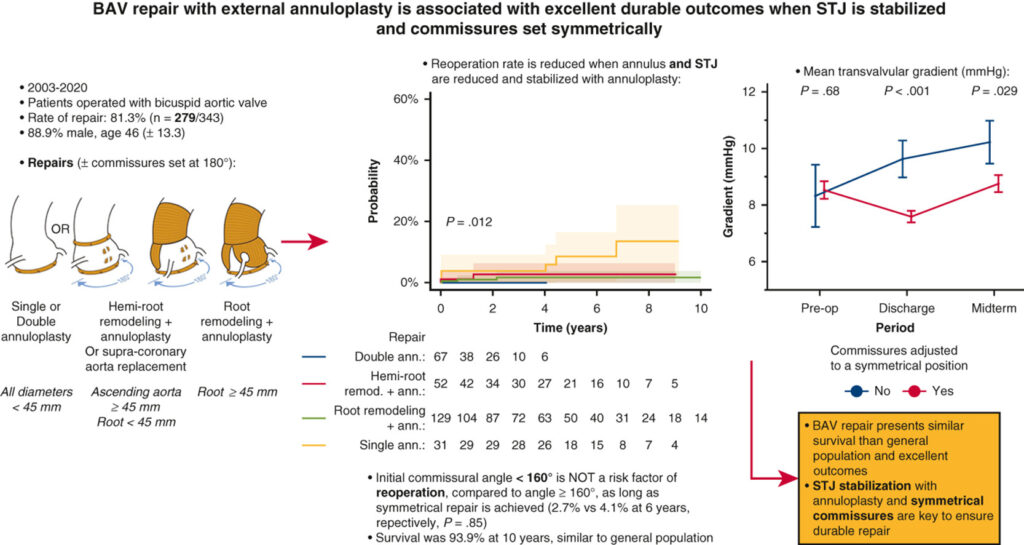
Outcomes of Bicuspid Valve Repair Are Improved by Sinotubular Junction and Annular Reduction and Stabilization Through External Annuloplasty
Objective
We studied the long-term outcomes of bicuspid aortic valve (BAV) repair with external annuloplasty, according to aortic phenotype.
Methods
Between 2003 and 2020, all BAV patients who underwent surgery for aortic insufficiency (AI) and/or aneurysm were included. Repairs included isolated AI repair with subvalvular annuloplasty with or without sinotubular junction (STJ) annuloplasty (single or double), supracoronary aortic replacement (with or without hemi-root remodeling), and root remodeling with subvalvular external annuloplasty.
Results
Among 343 operated patients, the reparability rate was 81.3% (n = 279; mean age 46 ± 13.3 years). At 10 years (median follow-up: 3.42 years; interquartile range 1.1–5.8), survival was 93.9% (n = 8 deaths, similar to the general population), the cumulative incidence of reintervention was 6.2% (n = 10), AI > grade 2 was 5.8% (n = 9), and AI > grade 1 was 23.0% (n = 30).
BAV repair stabilizing both the annulus and STJ with annuloplasty, compared to repair without STJ stabilization (simple annuloplasty), showed a lower incidence of reintervention (2.6% vs 22.5%, P = .0018) and AI > grade 2 (1.2% vs 23.6%, P < .001) at 9 years.
An initial commissural angle <160° was not a risk factor for reintervention, compared to an angle ≥160°, if a symmetrical repair was achieved (2.7% vs 4.1% at 6 years, P = .85).
The multivariate model showed that the absence of STJ stabilization (odds ratio 6.7; 95% CI, 2.1–20; P = .001) increased AI recurrence, but not an initial commissural angle <160° (odds ratio 1.01; 95% CI, 0.39–2.63; P = .98).
Symmetrically adjusted commissures resulted in a lower transvalvular gradient, compared to asymmetrical repair (8.7 mm Hg vs 10.2 mm Hg, P = .029).
Conclusions
BAV repair, adapted to the aortic phenotype, is associated with excellent durable outcomes if the annulus and STJ are reduced and stabilized by external annuloplasty. A commissural angle <160° is not associated with reintervention if a symmetrical repair is performed.
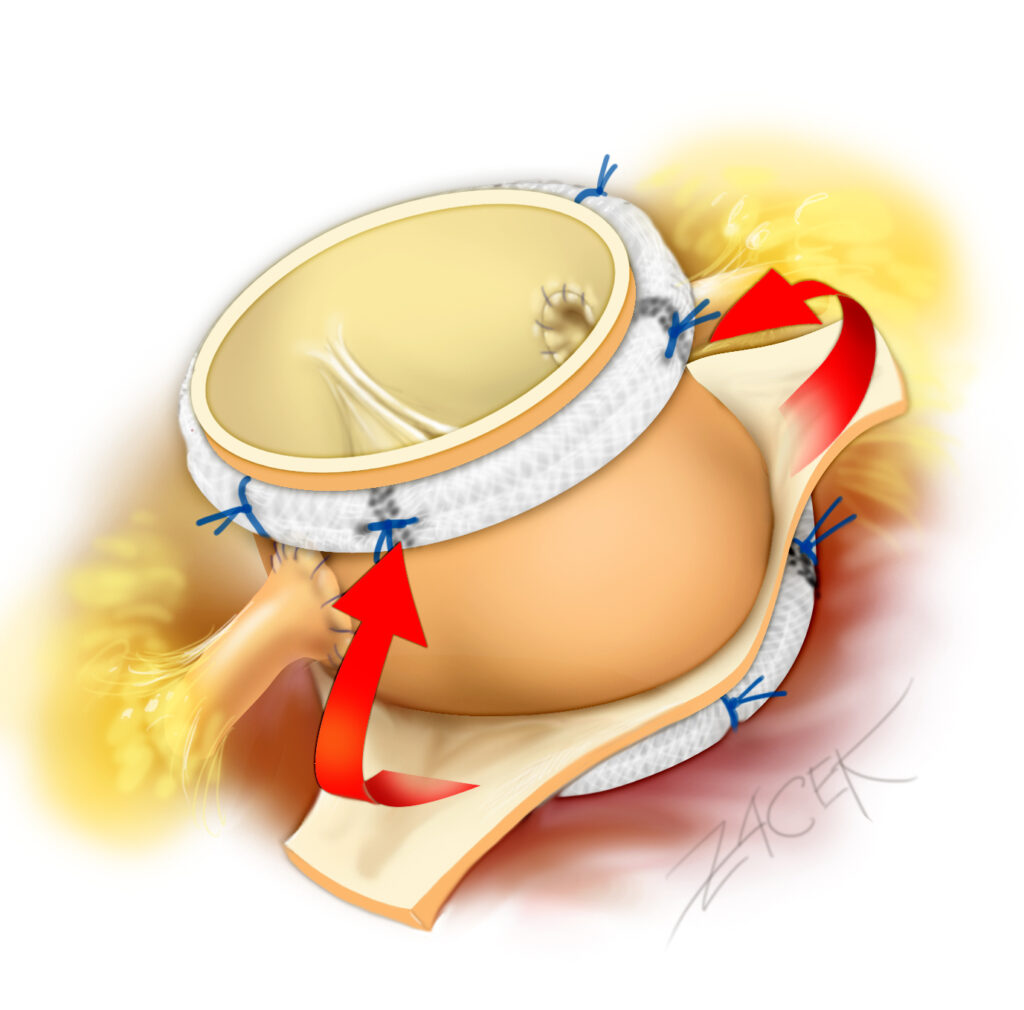
Graphical Abstract
Graphical abstract presenting the main methods, results, and conclusions of our study.
BAV: bicuspid aortic valve; STJ: sinotubular junction; Ann.: annuloplasty; Remod.: remodeling; AI: aortic insufficiency; OR: odds ratio; CI: confidence interval.
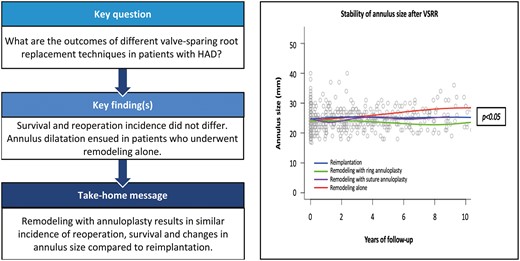
Outcomes of Aortic Valve-Sparing Surgery in Hereditary Aortic Diseases: Data from the AVIATOR Registry
OBJECTIVES
Root reimplantation is the preferred approach in patients with hereditary aortic diseases requiring valve-sparing root replacement. In recent years, root remodeling combined with annuloplasty has emerged as an alternative to reimplantation in the general population. The objective of this study was to evaluate the late outcomes of patients with hereditary aortic disease who underwent valve-sparing root replacement and to compare the different techniques.
METHODS
From the international AVIATOR (Aortic Valve Insufficiency and ascending aorta Aneurysm InternATiOnal Registry) registry, data were collected from 5 North American and European centers. Patients were divided into 4 groups according to the valve-sparing technique used: root reimplantation, root remodeling with ring annuloplasty, remodeling with suture annuloplasty, and remodeling alone.
The primary endpoints were freedom from aortic insufficiency (AI) ≥ grade 2 and freedom from aortic valve reintervention. Secondary endpoints were survival and changes in aortic annular dimensions over time.
RESULTS
A total of 237 patients were included in the study (reimplantation = 100, remodeling + ring = 76, remodeling + suture = 34, remodeling alone = 27). The majority of patients had Marfan syndrome (83%). Preoperative AI ≥ grade 2 was present in 41% of patients. Operative mortality was 0.4% (n = 1).
No difference was observed between the techniques in terms of postoperative AI ≥ grade 2 (P = 0.58), reintervention (P = 0.52), or survival (P = 0.59). However, the evolution of aortic annular dimensions differed significantly at 10 years (P < 0.05), with a divergence appearing as early as the 4th year after surgery.
CONCLUSIONS
Overall, valve-sparing root replacement is a safe and durable procedure in patients with hereditary aortic disease. However, root remodeling alone is associated with late annular dilation. The addition of annuloplasty, however, yields results comparable to reimplantation in terms of freedom from AI, reintervention, survival, and annular stability.
Bicuspid Valve Repair — Shraer et al., 2022
Bicuspid aortic valve (BAV), the most common congenital malformation, is almost always associated with annular dilation and ascending aortic pathology. Traditionally treated by valve replacement or Bentall procedure, valve repair nevertheless represents a promising option, capable of offering excellent long-term results.
Mustafa Zakkar, Emmanuel Lansac, and their team have developed a standardized approach to BAV repair, adapted to the proximal aortic phenotype. Three strategies are defined:
Dilated Root (>45 mm): root remodeling with expandable external annuloplasty.
Dilated Ascending Aorta (>45 mm) and Moderately Dilated Root (40–45 mm): tubular replacement with external annuloplasty.
Normal Root and Ascending Aorta (<45 mm): double annuloplasty (sub- and supravalvular at the STJ level).
The repair follows precise steps: alignment of the free edges of the cusps, evaluation of the effective cusp height (≥9 mm), and placement of external annuloplasty rings (Extra-Aortic Ring, Coroneo Inc.). A fundamental principle is to preserve the annulus/STJ ratio to ensure mechanical stability and optimal coaptation.
In a series of 191 patients, freedom from valve-related reintervention was excellent: 98% at 8 years for remodeling with a ring, and 100% for tubular replacement with a ring. In cases of isolated AI, double annuloplasty achieved 100% freedom from reintervention at 6 years, compared to 72.4% with a single subvalvular ring.
The technique also adapts to different BAV morphologies, particularly by symmetrizing the valve to obtain two equal cusps with 180° commissures. The authors emphasize that success relies on rigorous planning and surgical precision, with frequent use of intraoperative echocardiography.
Finally, although the results are excellent, the authors note that long-term follow-up still needs to be documented, particularly via the international AVIATOR registry.
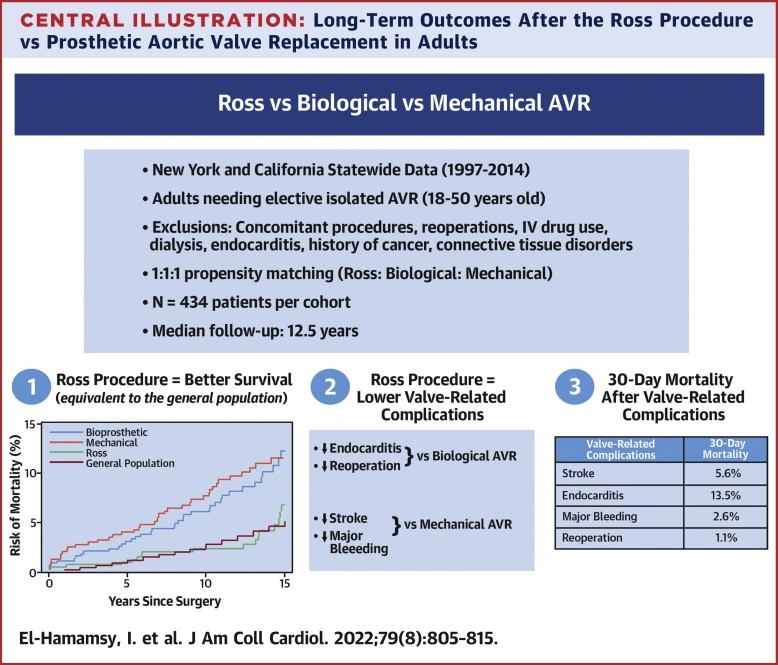
Propensity-Matched Comparison Between the Ross Procedure and Prosthetic Aortic Valve Replacement in Adults
Objectives
The objective of this study was to compare long-term outcomes after the Ross procedure versus biological and mechanical aortic valve replacement (AVR) in adults (aged 18 to 50 years) undergoing aortic valve surgery.
Methods
Mandatory databases from California and New York were queried between 1997 and 2014. Exclusion criteria included: ≥1 concomitant intervention, reoperations, infective endocarditis, intravenous drug use, hemodialysis, and out-of-state residency. Propensity score matching (1:1:1) was used, resulting in 434 patients per group. The primary endpoint was all-cause mortality. Secondary endpoints were stroke (CVA), major hemorrhage, reoperation, and endocarditis. Median follow-up was 12.5 years (IQR: 9.3–15.7 years).
Results
At 15 years, actuarial survival after the Ross procedure was 93.1% (95% CI: 89.1–95.7%), similar to that of the age-, sex-, and race-matched general US population. It was significantly lower after biological AVR (HR: 0.42; 95% CI: 0.23–0.075; p = 0.003) and after mechanical AVR (HR: 0.45; 95% CI: 0.26–0.79; p = 0.006). At 15 years, the Ross procedure was associated with a lower cumulative risk of reintervention (p = 0.008) and endocarditis (p = 0.01) than biological AVR. Conversely, at 15 years, the Ross procedure was associated with a higher cumulative incidence of reoperation (p < 0.001), but lower risks of stroke (p = 0.03) and major hemorrhage (p = 0.016) than mechanical AVR. Thirty-day mortality after valve-related complications was lowest after reintervention.
Conclusions
In young adults, the Ross procedure is associated with better long-term survival and greater freedom from valve-related complications, compared to prosthetic AVR. This confirms the idea that a living valve substitute in the aortic position translates into clinically superior outcomes.

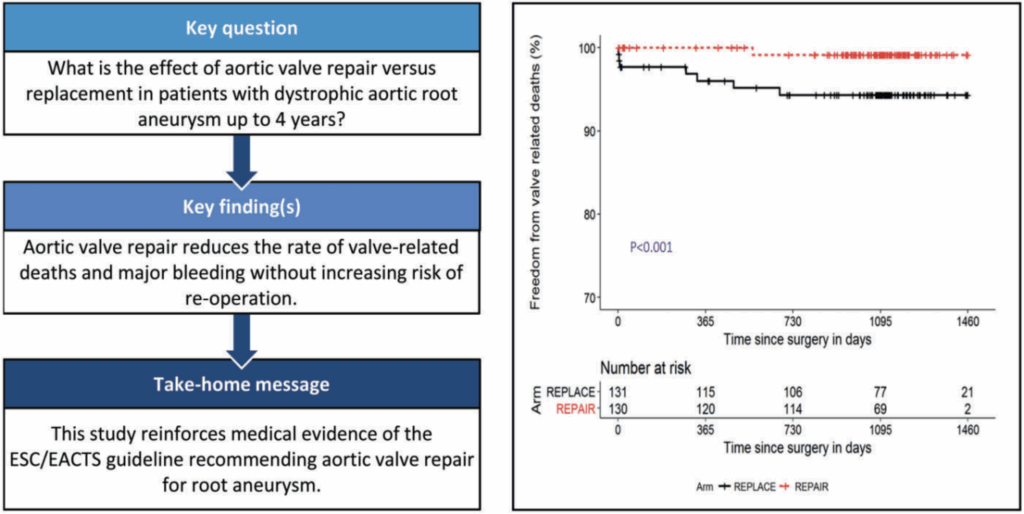
Aortic Valve Repair versus Mechanical Valve Replacement for Root Aneurysm: The Multicenter CAVIAAR Study
Bicuspid aortic valve (BAV), the most common congenital malformation, is almost always associated with annular dilation and ascending aortic pathology. Traditionally treated by valve replacement or Bentall procedure, valve repair nevertheless represents a promising option, capable of offering excellent long-term results.
Mustafa Zakkar, Emmanuel Lansac, and their team have developed a standardized approach to BAV repair, adapted to the proximal aortic phenotype. Three strategies are defined:
Dilated root (>45 mm): root remodeling with expandable external annuloplasty.
Dilated ascending aorta (>45 mm) and moderately dilated root (40–45 mm): tubular replacement with external annuloplasty.
Normal root and ascending aorta (<45 mm): double annuloplasty (sub- and supra-valvular at the STJ level).
The repair follows precise steps: alignment of the free edges of the cusps, evaluation of the effective cusp height (≥9 mm), and placement of external annuloplasty rings (Extra-Aortic Ring, Coroneo Inc.). A fundamental principle is to preserve the ring/STJ ratio to ensure mechanical stability and optimal coaptation.
In a series of 191 patients, freedom from valve-related reintervention was excellent: 98% at 8 years for remodeling with a ring, and 100% for tubular replacement with a ring. In cases of isolated AI, double annuloplasty achieved 100% freedom from reintervention at 6 years, compared to 72.4% with a single subvalvular ring.
The technique also adapts to different BAV morphologies, particularly by symmetrizing the valve to obtain two equal cusps with 180° commissures. The authors emphasize that success relies on rigorous planning and surgical precision, with frequent use of intraoperative echocardiography.
Finally, although the results are excellent, the authors note that long-term follow-up still needs to be documented, particularly via the international AVIATOR registry.